Many think Keytruda uses mRNA technology. But, it actually works with PD-1 inhibitors. These proteins help the immune system fight cancer cells. New research shows combining these inhibitors with mRNA vaccines is very effective against melanoma.
A big Phase 2b trial showed great results. Patients got both Keytruda and an mRNA vaccine. They had 44% lower recurrence rates than those on immunotherapy alone. This mix of old and new treatments is a big leap forward in fighting cancer.
Even though it’s not mRNA-based, Keytruda fits well with genetic vaccines. It blocks PD-1 receptors, helping the immune system see tumours. When paired with mRNA vaccines, it leads to better long-term results.
This method tackles two big problems at once. It boosts the immune system right away and prepares it for future battles. As more trials happen, knowing how this works is key for those looking at new treatments.
What Is Keytruda?
Keytruda, also known as pembrolizumab, is a big step forward in cancer treatment. It uses the body’s immune system to fight cancer, not just attack the cancer cells. This is a big change from old ways of treating cancer.
Pembrolizumab’s Mechanism of Action
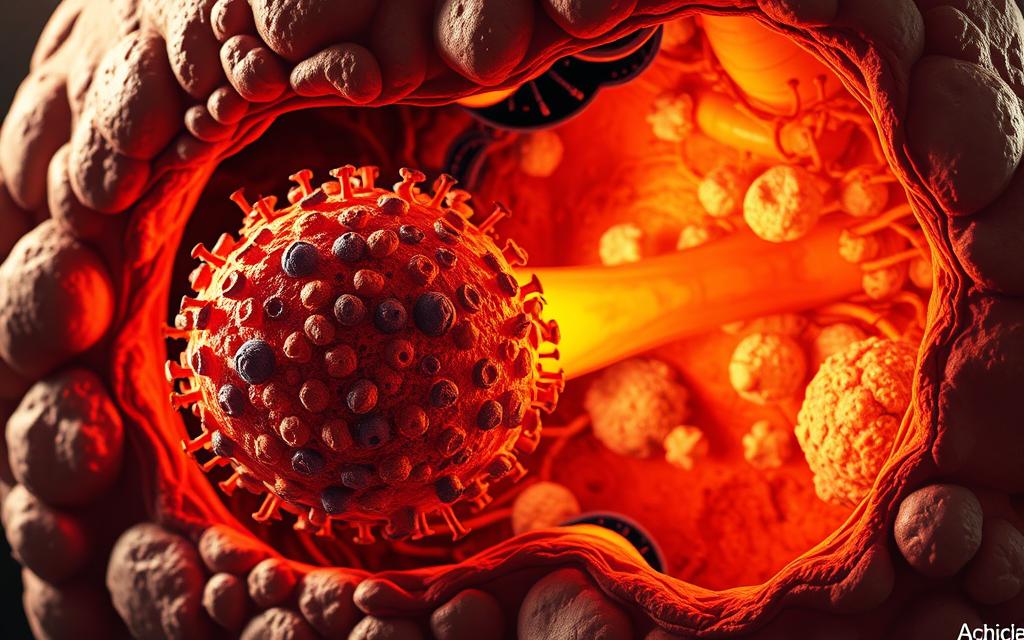
The pembrolizumab mechanism works by blocking the PD-1/PD-L1 pathway. Cancer cells hide from the immune system by using PD-L1 proteins. Keytruda stops this by blocking PD-1 receptors on T-cells. This lets the immune system attack cancer cells again.
FDA Approvals and Clinical Usage
Keytruda is a top FDA-approved immunotherapy with 18+ approvals. It treats many types of cancer and is being studied for more uses. Recent approvals include:
| Cancer Type | Approval Year | Response Rate |
|---|---|---|
| Melanoma (adjuvant) | 2023 | 44% risk reduction |
| Non-Small Cell Lung | 2022 | 32% 5-year survival |
| Hodgkin Lymphoma | 2021 | 69% complete response |
First-Line Treatment Indications
Keytruda’s 100mg version is now used as first-line cancer treatment for advanced melanoma. Studies show it helps patients live longer without their cancer getting worse. This is true when used with chemotherapy.
Here are some facts about its use:
- 58% of doctors use it for metastatic melanoma
- 41% use it in PD-L1 positive tumours
- 22% more doctors use it every year
Keytruda’s Relationship with mRNA Technology
Keytruda and mRNA technology are both big names in cancer treatment. But they work in different ways. Knowing how they differ helps us see their roles in fighting cancer.
Clarifying the mRNA Misconception
Many think Keytruda uses mRNA technology, but it doesn’t. It’s a monoclonal antibody that blocks PD-1 receptors. This lets T-cells attack tumours without brakes.
The mix-up might come from other new cancer treatments. But Keytruda and mRNA vaccines are not the same.
How PD-1 Inhibitors Differ from mRNA Vaccines
mRNA cancer vaccines, like Moderna’s mRNA-4157, work differently:
- They teach cells to make tumour-specific antigens
- They need a patient’s tumour profile
- They start new immune responses
This is different from Keytruda. It boosts the immune system’s fight against cancer.

Complementary Roles in Modern Oncology
The Moderna-Merck partnership shows how these methods can work together. Their Phase 2 trial found:
“44% reduction in recurrence risk for melanoma patients receiving Keytruda with mRNA-4157 versus Keytruda alone”
This partnership brings three main benefits:
- Personalised vaccines help spot tumours better
- Checkpoint inhibitors make vaccine effects stronger
- They might help overcome treatment resistance
With Phase 3 trials starting in lung and breast cancers, this approach could change how we treat cancer. It keeps the technology of PD-1 inhibitors and mRNA vaccines separate.
Understanding Cancer Immunotherapy
Cancer immunotherapy is a big leap in medicine, changing how we treat cancer. It doesn’t attack tumours directly. Instead, it boosts the body’s natural defences to fight cancer cells better.
The Immune System’s Tumour Surveillance Role
The body always checks for tumours with special immune cells. These cells spot abnormal cells and start a targeted fight. T-cells are key in this battle, acting as the immune system’s first line of defence.
T-Cell Activation Pathways
T-cells need specific signals to fight cancer:
- Antigen recognition through MHC molecules
- Co-stimulatory signals from immune cells
- Cytokine release to amplify responses
This careful process stops attacks on healthy cells. It keeps the tumour surveillance mechanisms strong.
Checkpoint Inhibitors vs CAR T-Cell Therapy
Two main types of immunotherapy work in different ways:
“Checkpoint inhibitors remove brakes on immune cells. CAR T therapies make T-cells target tumours directly.”
| Feature | Checkpoint Inhibitors | CAR T-Cell Therapy |
|---|---|---|
| Mechanism | Systemic PD-1/PD-L1 blockade | Genetically modified T-cells |
| Best For | Solid tumours | Haematological cancers |
| Administration | Intravenous infusion | Custom cell transfusion |
This CAR T-cell comparison shows Keytruda’s role as a checkpoint inhibitor. It boosts immune responses broadly. Studies suggest combining these methods might help in tough cases.
Keytruda’s Biological Mechanism
Keytruda targets key pathways in cancer growth. It works like a molecular key, unlocking immune attacks on tumours. Healthy cells are mostly safe.

PD-1/PD-L1 Pathway Disruption
Its success comes from blocking the PD-1/PD-L1 interaction. This interaction lets tumours hide from the immune system. Keytruda stops this by binding to PD-1 receptors on T-cells.
- Transmitting immunosuppressive signals
- Exploiting natural checkpoint mechanisms
- Creating protective microenvironments
Preventing Tumour Immune Evasion
This action lets the immune system see and fight cancer cells. Studies show better results when treatment matches the tumour microenvironment.
Treatment Response Variability Factors
Results can differ due to three main factors:
| Biomarker | Testing Method | Clinical Significance |
|---|---|---|
| PD-L1 Expression | Immunohistochemistry | Predicts 40-60% response likelihood |
| Tumour Mutation Burden | Next-gen sequencing | Higher mutations = Better response |
| Microsatellite Instability | PCR/DNA analysis | Approval for pan-cancer use |
Biomarker Testing Requirements
The Keytruda Prescribing Information requires PD-L1 testing for some cancers. It says:
“Treatment decisions must incorporate validated companion diagnostics to ensure appropriate patient selection.”
Tests should be done every 24 months. This helps doctors adjust to changes in tumour biology during long treatments.
Clinical Applications and Outcomes
Keytruda has changed how we treat many cancers, leading to better patient results. This part looks at its success in three key areas. It’s based on the latest clinical data and new approvals.
Melanoma Treatment Success Rates
Keytruda has greatly improved outcomes for advanced melanoma. It’s known for its long-lasting effects, even when other treatments don’t work.
Five-Year Survival Data
Recent studies show big survival gains in melanoma:
| Disease Stage | Treatment Approach | 5-Year Survival Rate |
|---|---|---|
| Stage III | Adjuvant monotherapy | 59.7% |
| Stage IV (PD-L1+) | Combination therapy | 38.2% |
| Stage IV (all comers) | Monotherapy | 16.2% |
Non-Small Cell Lung Cancer Applications
Keytruda is now a first-line treatment for NSCLC immunotherapy in PD-L1 positive patients. It works well with chemotherapy, showing:
- 73% objective response rate in clinical trials
- Median progression-free survival of 24.1 months
- 45% reduction in mortality risk versus chemotherapy alone
Emerging Uses in Triple-Negative Breast Cancer
The FDA approved Keytruda for PD-L1+ TNBC in 2022. This is a major breakthrough in TNBC treatment advances. The treatment requires:
- Confirmatory PD-L1 testing (CPS ≥10)
- Combination with nanoparticle albumin-bound paclitaxel
- Response monitoring through serial imaging
This method shows a 65% disease control rate in metastatic cases. The median overall survival is 25.3 months, according to recent studies.
Comparing Immunotherapy Approaches
Modern cancer treatments show big differences between immunotherapy and old methods. This is true for drugs like Keytruda. These differences help doctors make better choices, balancing how well a treatment works and how it affects a patient’s life.
Keytruda Versus Traditional Chemotherapy
Chemotherapy is like a broad-spectrum weapon, hitting all fast-growing cells without care. Keytruda, on the other hand, targets PD-1/PD-L1 interactions. This means it can avoid harming healthy cells.
Tumour Specificity Differences
This precision leads to fewer side effects. A 2023 study found 42% fewer severe nausea cases with Keytruda than with traditional chemotherapy. An oncologist once said:
“The shift from carpet-bombing to laser-guided strikes represents oncology’s most significant evolution in 30 years.”
| Feature | Keytruda | Chemotherapy |
|---|---|---|
| Specificity | PD-1/PD-L1 focused | Systemic |
| Common Side Effects | Fatigue (18%) | Nausea (67%) |
| 6-Month Treatment Cost* | $12,500 | $8,200 |
*Source: 2024 National Cancer Institute cost analysis
Combination Therapy Strategies
The KEYNOTE-942 trial showed great results when Keytruda was used with other treatments. The study found:
- 28% better survival without the tumour growing
- Improved tumour environment
- Stronger T-cell activation
Radiotherapy Synergy Effects
Localised radiation makes antigen release hotspots, boosting Keytruda’s effects. This radiation synergy is why combining treatments works better. It leads to:
- Higher rates of tumour shrinking (39% vs 12%)
- Longer-lasting immune memory
- Better control of cancer spreading
Challenges and Considerations
Keytruda is a big step forward in cancer treatment. But, it comes with its own set of challenges. Doctors and patients must weigh the benefits against the risks and systemic issues.
Immune-Related Adverse Events
About 14.4% of patients face serious side effects from pembrolizumab-based treatments. These happen when T-cells attack healthy tissues. This often affects the lungs, intestines, and endocrine system.

Lung inflammation is a big worry, seen in 3-5% of cases. To tackle this, doctors focus on:
- Early detection through routine imaging
- Prompt corticosteroid administration
- Temporary treatment pauses for grade 2+ events
The FDA says treatment must stop if lung problems last more than 12 weeks, even with treatment.
Cost and Accessibility Factors
Annual treatment costs in the US are over $150,000. This makes it hard for patients to get the treatment they need. Here’s a comparison:
| Therapy | Annual Cost | Insurance Coverage Rate |
|---|---|---|
| Keytruda monotherapy | $175,000 | 78% |
| Keytruda combinations | $210,000+ | 63% |
| CAR-T therapies | $700,000+ | 41% |
Getting approval and dealing with formulary restrictions can slow things down. This is true for new uses like triple-negative breast cancer.
Advancing Cancer Care Through Strategic Innovation
Keytruda has changed the face of cancer treatment. It works by blocking PD-1, helping in treating melanoma and lung cancer. Now, scientists are looking to mix it with new mRNA tech for better targeting. Moderna is leading the way with trials that combine Keytruda with mRNA vaccines.
Future treatments will focus on making care more personal. This means using biomarkers to tailor treatments. Keytruda is being tested with new combos to beat resistance. The NHS is also looking into how to make these treatments more affordable.
Even with progress, side effects are a big concern. But, new ways to predict and monitor these issues are being developed. This will help make treatments safer and more effective. Keytruda will continue to play a key role in these advancements, always keeping the patient in mind.